PHOTONIC FRONTIERS: BIOPHOTONICS: Adaptive optics examines the eye
Biophotonic examination of the eye might seem straightforward because it evolved to transmit light. However, as David Williams of the University of Rochester (Rochester, NY) observed in a review paper, "It has never been easy to peer inside the living eye."1 The pupil offers only a small and sometimes cloudy window on the interior of the eye, and the retina reflects only 0.001 to 0.00001 of the incident light back through the pupil. Internal aberrations limit resolution so external instruments can't see individual cells, and many studies of visual function had to be done with retinal tissue removed from the eye.
Now new photonic techniques are making optical examination of the living eye easier. Optical coherence tomography (OCT) records the retina's microstructure in situ, in the offices of ophthalmologists, helping them to accurately diagnose the causes of their patients' vision problems. Adaptive optics can compensate for the eye's internal aberrations, recording images that reveal individual photoreceptors in the retina both for clinical studies of eye disease and for fundamental research on vision.
Looking inside the eye
The standard instrument used for visual examination of the eye is a refined version of the ophthalmoscope invented in 1850 by Hermann von Helmholtz. For an optically perfect eye with a normal pupil aperture, the diffraction-limited resolution is 1.4 μm, sufficient to resolve the smallest photoreceptors on the retina. However, eyes have internal aberrations that make it impossible to resolve either rods or cones in the living eye. Optical coherence tomography, invented in the 1980s, overcomes those aberrations in the axial dimension to record the retina's internal structure, but it does not achieve the same resolution across the retina.
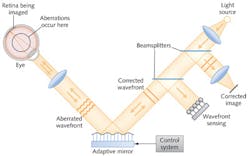
Adaptive optics can compensate for all aberrations in the eye by measuring the internal aberration and adjusting the wavefront of light entering the eye. However, Williams soon encountered a showstopper. As he wrote in his review, "I will never forget the $1 million price tag on the only deformable mirror available when I first contemplated building an adaptive optics ophthalmoscope." He had to wait years for the price to come down more than an order of magnitude before he could afford a deformable mirror. But when he did, the technology lived up to its promise, imaging single cells in the retina and opening up new possibilities for vision research and ophthalmology.
Figure 1 shows a closed-loop adaptive optical system for retinal imaging. Light from an external source, reflected from the retina, is focused onto sensors that measure its aberrations and use that information to adjust the shape of the adaptive mirror to focus light more sharply. The system adapts continually to compensate for changing aberrations. In October 2012, Williams told the Optical Society's Frontiers in Optics conference that such a system could reduce refractive errors by about a factor of 10, compensating both for standard aberrations correctable by external optics and for nonstandard aberrations. That allows lateral resolution both for cones, about 5 μm across, and for rods, only 2 μm.
Adding adaptive optics also improves other instruments. Austin Roorda, now at the University of California-Berkeley (Berkeley, CA), used it to improve lateral resolution of a scanning laser ophthalmoscope to less than 2 μm, although its 60 μm axial resolution cannot match that of OCT. Adaptive optics also can improve the resolution of OCT to less than 3 μm both laterally and axially.2
Retinal imaging
Imaging the retina poses major challenges, including the small aperture of the pupil, and the strong light scattering and poor fixation often found in diseased eyes. But the dramatic improvement in resolution can provide objective data on the retina that were never before available. Traditional measurements of visual acuity can miss serious degradation because the human visual system is surprisingly resilient to damage such as the loss of photoreceptors. "You can have visual acuity of 20/20 when 50% of the cones are gone," says Roorda, so imaging receptors can spot problems missed by standard eye exams.
Retinal imaging also can play a vital role in assessing the treatment of eye disease. "Because we have a microscopic view of the retina, we can view the progress of retinal disease," better than by measuring changes in visual acuity. With adaptive optics, Roorda says, "we can count cells, and see degeneration" much faster. Comparing cone counts during drug tests could yield definitive results in as little as two to three years, faster than acuity tests, reducing costs and speeding valuable drugs to market. With Katherine Talcott and Jacque Duncan of the University of California-San Francisco (San Francisco, CA), Roorda detected change in the retinas of patients with the degenerative disease retinitis pigmentosa within two years using adaptive optics, although acuity tests revealed no difference.3
Vision research is also benefiting. High-resolution images reveal that the 1.2 million ganglion cells on the surface of the retina are divided into 17 different classes, with long axions that extend to the brain and dendrites reaching out to hundreds or thousands of other cells. "Each of these retinal cells tiles the whole visual surface, as if they are all independent pathways" for processing visual information, Williams says. He and Bill Merigan of Rochester have made ganglion cells fluoresce when they carry electrical signals, allowing them to figure out what they are doing in living eyes and monitor their activity for years.4 Much remains to be learned about ganglion cells and their functions, and they are important clinically because they are affected by glaucoma.
Vision research
The ability of adaptive optics to focus on a single photoreceptor in a living eye opens a new window for vision researchers, who have long been limited to studying collective effects of light on many photoreceptors. One of the first applications in vision research was to map the distribution of the red, green, and blue cones in normal eyes. The distributions turned out to be largely random but with the ratios of red to green cones varying by a factor of 40; Fig. 2 shows the differences among various eyes.Examination of single photoreceptors is also improving our understanding of color vision, which combines inputs from red, green, and blue cones to give us a rich sense of hue. Looking at individual cones and other retinal cells shows how the process works at a cellular level in the living eye. Thus they can yield information on the whole visual system, spanning the cones, the brain, and all the cells in between, not available from studies of excised retinas. "A lot of color information processing is done in the retina, before the signals are sent to the brain," says Roorda.5
Stimulating individual cones in the living eye with different wavelengths yielded surprising results. Simple models of color vision predict that each type of cone would produce its own response, so a yellow laser line at 580 nm would look red to the brain because it strongly stimulated the red cone and only weakly stimulated the green. However, when Heidi Hofer of Rochester stimulated single cones in volunteers with different wavelengths, she found they reported seeing seven different colors, not the expected red, green, and blue.6
Another surprise came from adaptive-optical imaging of the eyes of humans with only two types of cones, making them red-green color blind. Different genes have been linked to the trait, but their effects had been considered similar until Joe Carroll used adaptive optics to profile cone distribution in affected people. He found that cone mosaics of people with one genetic pattern look normal although they have only two cone types, but those of people with a different pattern have gaps in their cone fields, where the missing cone type failed to form, as shown in Fig. 3.7Outlook
Adaptive optics is becoming a powerful tool for vision research, making it possible to study the operation of single photoreceptors in a living eye, integrated with the visual circuitry of the brain and retina. That's essential for understanding how the vision system works. It has already yielded new insight into the mechanisms of color vision, and promises a quantitative assessment of retinal degradation that is far more sensitive than current clinical techniques.
The high cost of adaptive optics poses a formidable obstacle for clinical applications. The first success could be in taking advantage of high-sensitivity direct retinal imaging to speed clinical trials of new drugs and treatments, reducing trial costs and bringing drugs to market faster. Further reductions in component cost and improvements in system performance could lead to new clinical instruments for assessing vision, monitoring changes in the eye, and helping preserve vision, building on the success of current imaging technology-including ophthalmological OCT systems.
REFERENCES
1. D. Williams, "Imaging single cells in the living retina," Vision Research, 51, 1379–1396 (2011); doi:10.1016/j.visres.2011.05.002.
2. L. Yin and D.R. Williams, "Adaptive optics" in The retina and its disorders, J.C. Behearse and D. Bok (eds.), Academic Press (2010).
3. K.E. Talcott et al., "Longitudinal Study of Cone Photoreceptors during Retinal Degeneration and in Response to Ciliary Neurotrophic Factor Treatment," Investigative Ophthalmology & VisualScience, 52, 5, 2219–2226 (April 2011).
4. Y. Geng et al., "Adaptive optics retinal imaging in the living mouse eye," Biomed. Opt. Expr., 3, 715–734 (April 2012).
5. A. Roorda, "Adaptive optics for studying visual function: A comprehensive review," J. Vision, 11, 5:6, 1–21 (2011); doi:10.1167/11.5.6.
6. H. Hofer, B. Singer, and D.R. Williams, "Different sensations from cones with the same photopigment," J. Vision, 5, 5, 444–454 (2005); doi:10.1167/5.5.5.
7. J. Carroll et al., "Functional photoreceptor loss revealed with adaptive optics: An alternate cause of color blindness," Proc. Natl. Acad. Sci. V, 101, 8461–8466 (2004).
8. J. Carroll et al., "Recent advances in retinal imaging with adaptive optics," Opt. and Photon. News, 16, 36–42 (January 2005).

Jeff Hecht | Contributing Editor
Jeff Hecht is a regular contributing editor to Laser Focus World and has been covering the laser industry for 35 years. A prolific book author, Jeff's published works include “Understanding Fiber Optics,” “Understanding Lasers,” “The Laser Guidebook,” and “Beam Weapons: The Next Arms Race.” He also has written books on the histories of lasers and fiber optics, including “City of Light: The Story of Fiber Optics,” and “Beam: The Race to Make the Laser.” Find out more at jeffhecht.com.

