FIBER-OPTIC MICROSCOPY: Bent on disease detection: Fiber optics makes miniature microscopy more flexible
While fiber optics is well known in the realm of light sources, fiber-optic microscopy is lesser known. But the bendable nature of optical fiber provides significant benefit for microscopy: Fiber allows relatively easy access to regions of interest, and thus extends the reach of microscopic imaging.
Optical fiber can be applied in various ways for microscopy. As one example, Timothy J. Muldoon, assistant professor of biomedical engineering at the University of Arkansas in Fayetteville, turned a conventional microscope into a fiber-optic instrument. The system directs light through the objective lens, which then passes into an optical fiber bundle that gets positioned over the sample. This system uses a coherent—or image guide—fiber bundle, in which the packed set of fibers is arranged the same way on both ends. This creates a small, flexible conduit that transmits a pixelated image of the sample.
The resolution of such a system depends on the diameter of the fibers. Muldoon's microscope uses fibers 3 μm in diameter—about the size of a nucleus. "We can place the bundle in contact with a tissue," he says, "and get spatial resolution at the cellular level, even without any optics at the end of the bundle at the tissue." The complete probe is usually 1–2 mm in diameter, which determines the overall field of view.
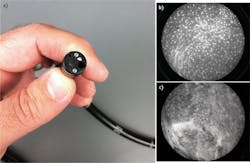
Muldoon calls this a very simple system. "It's small, flexible, and it can be guided to various tissues." For example, Muldoon uses it to explore a variety of tissues in vivo (see Fig. 1). Nonetheless, Rebecca R. Richards-Kortum—the Stanley C. Moore Professor of Bioengineering at Rice University (Houston, TX), and a pioneer in this technology—points out some challenges with fiber-optic microscopes. "Resolution is not yet the same as for standard histology, and penetration depth is limited," says Richards-Kortum. "So it is not a solution that works in all cases."
Novel by necessity
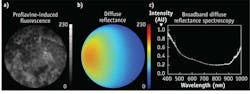
In many situations, scientific needs drive innovation. To some extent, that happened with Richards-Kortum. She says, "I was doing a lot of microscopy of tissue biopsies and wanted to be able to get similar image quality without the need to remove tissue." That triggered her interest in fiber-optic microscopy. Consequently, she developed a way to use fiber-optic microscopy to image epithelial tissue in vivo (see Fig. 2). This technology lets a researcher find tissue that looks the most abnormal, and then perform a conventional biopsy of that spot. In describing the fiber-optic procedure, Richards-Kortum says, "It can be painless and inexpensive."Muldoon earned his Ph.D. in Richards-Kortum's lab at Rice, and he envisions many applications of this technology. For one thing, a fiber-optic microscope could be developed as a handheld probe used by a dentist or oral surgeon to map out possibly cancerous lesions. "Abnormal cellular structure can then guide a surgeon to the spots that should be biopsied," Muldoon says.
Similar technology could also image even deeper in the body. As an example of this, Muldoon discusses Barrett's metaplasia, in which glandular tissue replaces the surface epithelium. "About 1 percent of the people who have this get esophageal adenocarcinoma, which is very bad," Muldoon says. "If you use our technology, a clinician can survey a much broader area during an endoscopic procedure and produce live histology to target where biopsies are needed." In fact, Richards-Kortum says, "We are just beginning a multi-center trial in China to look at whether fiber-optic microscopy can improve detection of esophageal precancer." She adds, "We are also examining whether this is a cost-effective solution for areas that can't afford traditional screening approaches."
Expanding the availability of screening makes up a crucial opportunity for fiber-optic microscopy to advance public health around the world. "Many areas lack both the human resources and physical infrastructure for standard histologic diagnosis," Richards-Kortum says. "Fiber-optic microscopy—because of its low cost and automated interpretation—may allow these places to leapfrog the need for this infrastructure."
Easy access
To spread the use of fiber-optic microscopy to clinicians around the world, devices must be available commercially. Most people won't make devices like Richards-Kortum and Muldoon do, but other options exist.
For instance, Mauna Kea Technologies, headquartered in Paris, makes Cellvizio, which it calls a confocal laser endomicroscope. In this device, a fiber-optic bundle—composed of thousands of fibers, each less than 2 μm in diameter—replaces the objective lens. In addition, optics at the end of the fibers can focus the light into a tissue. François Lacombe, the company's chief innovation officer, says "The depths can range from 0 to 100 micrometers, depending on the model."
The number of fibers in the bundle varies with the specific Cellvizio model, and ranges from 10,000-30,000. "The bundle itself is less than 0.7 millimeters in diameter," says Lacombe. "Together with the sheath—which protects it during use, but also during sterilization or disinfection—and the tiny distal optics, the complete optical probe can be as small as 1 millimeter in diameter, which makes it compatible with 19G needles, and thus makes it possible to image inside solid organs such as pancreas."
Lacombe and his colleagues always planned to direct this device at medical applications. He says, "Cellvizio was designed, since day one, to provide physicians with microscopic images of tissues that are suspected to host the very early stages of most of cancers, such as of the epithelium of the gastrointestinal tract, pulmonary airways, or the urinary tracts."
Eventually, Lacombe hopes that such 'optical biopsies' can be used on "any imaginable area in the entire body—kidney, liver, brain, many domains."
Getting the most from any fiber-optic microscope depends on more than the optics. "You can look at quantitative image analysis and computer diagnostics," Muldoon explains. "Overall, this technology can help a surgeon visualize a larger area more rapidly and in a more objective way." Hopefully, these advances will lead to more objective diagnoses at very early stages of disease and huge benefits in the outcome of treatments.
Fiber-optic microscopy aids colorectal cancer surgery
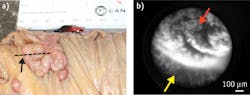
In 2014, more than 50,000 Americans died from colorectal cancer, according to estimates from the U.S. National Cancer Institute. Surgical procedures can treat some instances, but especially for this form of cancer, removing as little healthy tissue as possible (while resecting all of the cancerous tissue) improves the odds of biological function after the procedure. To help with this, Muldoon is developing a fiber-optic microscope that can distinguish diseased from healthy tissue during the surgery.
"This device can be used in endoscopically guided surgery or intraoperatively during conventional surgery to map tumor margins and regions not visible by eye," Muldoon explains. "It doesn't replace existing procedures, but complements them."
Although this device's field of view only covers 1–2 mm, the instrument tiles images together over time. "It's almost like you 'paint' an area that you want to investigate, and then the images get stitched together," Muldoon says. "This overcomes the physical limitations of the probe."In ongoing early clinical trials on this device, Muldoon hopes to identify structural markers that can be used in quantitative image analysis and correlated with specific pathologies, like a particular cancer. "We'll build an image library and correlate the histology with the diagnosis," Muldoon says.
A spectral tweak might reveal even more with this device. Using the same probe and adding spectroscopy, Muldoon can look below a tissue's surface. "It's still a flexible probe of the same size, but it uses spectroscopy to look at different depths. It will add even more information to the surface imaging," Muldoon says. "The spectroscopy adds a biochemical or functional element to the structural information."
Muldoon sees this technology helping pathologists. "In the operating room," he says, "it won't be a final diagnosis, but it will help guide the surgical approach."
Mike May | Contributing Editor, BioOptics World
Mike May writes about instrumentation design and application for BioOptics World. He earned his Ph.D. in neurobiology and behavior from Cornell University and is a member of Sigma Xi: The Scientific Research Society. He has written two books and scores of articles in the field of biomedicine.