Fluorescence imaging could enable more effective ovarian cancer removal
Knowing that ovarian cancer is one of the most difficult types of cancer to treat, researchers at the Massachusetts Institute of Technology (MIT; Cambridge, MA), working with surgeons and oncologists at Massachusetts General Hospital (MGH; Boston, MA), have developed a way to improve the accuracy of ovarian cancer surgery (debulking). Using a fluorescence imaging system, they were able to find and remove tumors as small as 0.3 mm during surgery in mice. Mice that underwent this type of image-guided surgery survived 40% longer than those who had tumors removed without the guided system.
The system allows for real-time information about the size, depth, and distribution of tumors, says Angela Belcher, the James Mason Crafts Professor of Biological Engineering and Materials Science at MIT, a member of the Koch Institute for Integrative Cancer Research, and the recently appointed head of MIT's Department of Biological Engineering.
Belcher and Michael Birrer, formerly the director of medical gynecologic oncology at MGH and now the director of the O’Neal Comprehensive Cancer Center at the University of Alabama at Birmingham, joined forces to work on this problem through the Bridge Project, a collaboration between the Koch Institute and Dana-Farber/Harvard Cancer Center. Belcher's lab has been developing a novel type of medical imaging based on light in the near-infrared (near-IR) spectrum. In a paper published in March 2019, she reported that this imaging system could achieve an unprecedented combination of resolution and penetration-depth in living tissue.
In the new study, Belcher, Birrer, and their colleagues worked with researchers at MIT Lincoln Laboratory to adapt near-IR imaging to help surgeons locate tumors during ovarian cancer surgery, by providing continuous, real-time imaging of the abdomen, with tumors highlighted by fluorescence. Previous analyses have shown that survival rates are strongly inversely correlated with the amount of residual tumor mass left behind in the patient during debulking surgery, but many ovarian tumors are so small or hidden that surgeons can't find them.
To make the tumors visible, the researchers designed chemical probes using single-walled carbon nanotubes that emit fluorescent light when illuminated by a laser. They coated these nanotubes with a peptide that binds to SPARC, a protein that is overexpressed by highly invasive ovarian cancer cells. This probe binds to the tumors and makes them fluoresce at near-IR wavelengths, allowing surgeons to more easily find them with fluorescence imaging.
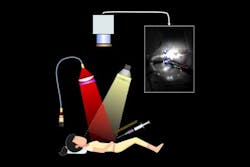
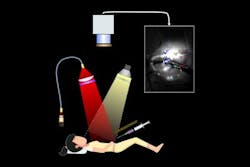
Researchers at MIT and MGH have developed an image-guided surgical system that could help surgeons better visualize and remove tiny ovarian tumors. Fluorescent carbon nanotubes are used as probes to bind to the tumors, making them easier to see. (Image courtesy of the researchers)
The researchers tested the image-guided system in mice that had ovarian tumors implanted in a region of the abdominal cavity known as the intraperitoneal space, and showed that surgeons were able to locate and remove tumors as small as 0.3 mm. Ten days after surgery, these mice had no detectable tumors, while mice that had undergone the traditional, non-image-guided surgery, had many residual tumors missed by the surgeon.
By three weeks after the surgery, many of the tumors had grown back in the mice that underwent image-guided surgery, but those mice still had a median survival rate that was 40% longer than that of mice that underwent traditional surgery.
"You can't have a patient in a CT machine or an MRI machine and have the surgeon perform this surgical debulking procedure at the same time, and you can't expose the patient to x-ray radiation for multiple hours of the long surgery. This optics-based imaging system allows us to do that in a safe manner," explains Neelkanth Bardhan, a Mazumdar-Shaw International Oncology Fellow at the Koch Institute.
For most ovarian cancer patients, tumor debulking surgery is followed by chemotherapy, so the researchers now plan to do another study where they treat the mice with chemotherapy after image-guided surgery, in hopes of preventing the remaining tiny tumors from spreading.
"We know that the amount of tumor removed at the time of surgery for patients with advanced-stage ovarian cancer is directly correlated with their outcome," Birrer says. "This imaging device will now allow the surgeon to go beyond the limits of resecting tumors visible to the naked eye, and should usher in a new age of effective debulking surgery."
Now that they have demonstrated that this concept can be successfully applied to imaging during surgery, the researchers hope to begin adapting the system for use in human patients.
The researchers also hope to deploy this type of imaging to monitor patients after surgery, and eventually to develop it as a diagnostic tool for screening women at high risk for developing ovarian cancer.
The researchers are now seeking FDA approval for a phase 1 clinical trial to test the imaging system in human patients. In the future, they hope to adapt the system for monitoring patients at risk for tumor recurrence, and eventually for early diagnosis of ovarian cancer, which is easier to treat if it is caught earlier.
Full details of the work appear in the journal ACS Nano.