A new view of robotic surgery
Designed to work with the magnetic-resonance imaging systems already integrated into operating rooms, a new type of robotic system takes a different approach to enhancing surgical vision.
By Dr. Garnette R. Sutherland, Jason W. Motkoski, Catherine O. Sutherland, and Alexander D. Greer
Advances in neurosurgery have paralleled technological development–particularly in terms of lesion localization and microsurgical technique–for many years. Incorporating robotic technology into the surgical imaging environment couples the human ability to predict based on past experience with the increased precision and accuracy of machines.1 It takes surgery “beyond the limits of the human hand,” to quote Intuitive Surgical (Sunnyvale, CA), maker of the endoscopic da Vinci instrument, the most widely used surgical robotic system (with more than 1000 installations).
But while da Vinci has had tremendous success in urologic surgery (particularly for prostate cancer removal) among other areas, such existing systems are not ideal for neurosurgery. Ideally, a neurosurgical robotic system would integrate with installed imaging systems, including the ubiquitous magnetic-resonance (MR) imaging machines that have already been successfully integrated into the operating room.2
A different approach to robotic surgery, neuroArm (developed in collaboration between the University of Calgary and MacDonald Dettwiler and Associates)is not an endoscopic system, but rather an image-guided robotic system capable of both stereotaxy (biopsy) and microsurgery.3 It is MR-compatible–meaning that it operates within an MR imaging machine.
For microsurgery, it transports MR images of the entire brain to the surgeon, who controls the robot at a workstation. Two high-definition cameras mounted to the surgical microscope provide a three-dimensional (3-D) view of the surgical site, transmitting optical imagery to two miniature monitor displays at the workstation.
For stereotactic procedures or stereotaxy, one arm is mounted on a platform within the magnet. In this configuration, the surgeon working at a workstation is able to obtain the biopsy during MR imaging. This is important because it provides direct confirmation that the sample has been acquired from the correct location and that the biopsy procedure has not resulted in an undesirable event.
System components
While MR compatibility empowers neurosurgery, it challenges system design, limiting the choice of component materials to those that are not ferromagnetic–for example, titanium, PEEK (polyetheretherkeytone), and Delrin, ceramics, or piezoelectrics. It is vital that MR image acquisition does not affect the robot and that the robot does not affect MR image quality.
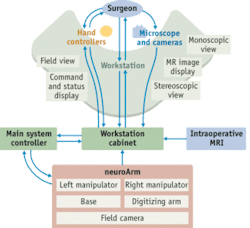
The setup includes two manipulators (arms) on a movable base platform, a workstation, and a system-control cabinet (see Fig. 1). A variety of visualization tools tie the system together. The manipulators have seven degrees of freedom (DOF) and are designed to hold a variety of standard surgical tools (see Fig. 2). Ultrasonic piezoelectric motors provide 100 nm resolution and have inherent braking characteristics in case power is lost. Sine/cosine 16-bit absolute encoders allow 0.05-degree accuracy and are used on the input and output of each joint to provide fault detection in the event that one encoder should fail. Antibacklash gears manufactured from titanium and machined to extremely tight tolerances allow smooth motion.
Custom six-axis, force/torque sensors provide feedback of tooltip forces in three translational DOF. Those located directly between the tool and end effector provide high-fidelity haptics to the hand controllers for enhanced surgical dissection. Such force feedback also provides a method by which dissection can be quantified, and thus, an ability to set limits on force exerted by the surgeon.
A standardized tool interface allows for roll and actuation while ensuring that the tool can not be accidentally disengaged. The design permits rapid tool exchange, minimizes disruption of surgical rhythm, decreases chance of tool damage, and allows draping to maintain sterility.
The mobile base serves as the positioning mechanism for the manipulators, the digitizing arm used for manipulator registration, and the surgical field camera. In stereotactic mode, the base is used to transfer one of the manipulators to a platform mounted inside the gradient insert of the magnet (see Fig. 3). Within the magnet, the manipulator and biopsy tool are registered to the MR images. A single camera was not able to capture all of the critical components simultaneously, so the system includes two MR-compatible cameras mounted on the platform that transmit images of the manipulator, surgical tool, and surgical site to the surgeon at the workstation. In this configuration, biopsy can be performed and the sample easily transferred out of the gradient aperture.
A 980 nm contact diode-laser system (Photomedex; Montgomeryville, PA) is currently being integrated with neuroArm. In contact laser surgery, the laser beam is contained within a sapphire tip at the distal end of the fiber, rather than passing directly out of the fiber. The light energy remains within the sapphire tip until contact is made with tissue. Penetration of the laser energy is less than 0.5 mm because the 980 nm wavelength is highly absorbed by the water in tissue, minimizing damage to adjacent structures. This wavelength is also absorbed by proteins, allowing coagulation of vessels up to 0.5 mm. When attached to the neuroArm tool interface, the surgeon is uniquely provided a laser with a sense of touch.
The view from the workstation
The sensory-immersive workstation is located in a room adjacent to the operating room (see Fig. 4). The workstation comprises two video monitors, two touch-screen computer displays, a stereoscopic display unit, and two force-feedback hand controllers.4 The leftmost monitor displays a 2-D image from the surgical microscope, while the rightmost monitor provides the field camera view. A Leica OH4 surgical microscope (Leica Microsystems (Schweiz); Heerbrugg, Switzerland), was modified to provide stereoscopic video output to the workstation. This microscope provides excellent optics and can be moved in the x, y, and z planes using a footswitch that is remotely located at the workstation.
The two touch-screen displays are located directly to the left and right of the surgeon. Magnetic-resonance images are uploaded onto the left touch-screen display and can be manipulated in either 2-D or 3-D and used for surgical planning. Such a display, together with virtual tool overlay, allows visualization of the lesion in relation to the tools from any chosen angle. This enhances surgical vision by providing knowledge of the location of structures outside the surgical corridor. The other touch-screen display shows a virtual representation of the manipulators, radio-frequency coil, and, when in stereotactic mode, the MR magnet with gradient insert. This display provides interactive rolling of the 3-D image, and includes command settings and robot status.
Two high-definition cameras (Ikegami Tsushinki Co.; Tokyo, Japan) mounted on the surgical microscope are used in microsurgery mode and they are the eyes of the surgeon at the workstation. They transmit to two miniature full-color displays (Rockwell Collins; Cedar Rapids, IA), providing the surgeon with a stereoscopic or 3-D view of the operative site. The two miniature full-color displays are currently being upgraded to high definition.
Two PHANTOM haptic hand controllers were altered with a stylus and actuator to better mimic conventional surgeon-tool motion and actuation. The stylus includes a finger-activated lever for tool actuation; has a strain-gauge switch for enabling or disabling the manipulators; and allows six DOF, position, and orientation. Two-way audio communication is supplied between the operating room personnel and surgeon. A microphone positioned adjacent to the surgical field provides the surgeon with the acoustics of surgical dissection.
Safety and precision
Safety in medical robotics is of considerable importance. For nueroArm, confirmation via additional hardware action is required for safety-critical software events, such as turning on power or enabling arm motion. In addition, the surgeon is able to define a virtual geometric region on the left touch-screen display, which can include the surgical corridor or anatomical structures to be avoided. When the surgeon reaches such a predefined boundary, the manipulators are not permitted to advance and force feedback is relayed to the surgeon’s hand, creating no-go zones. This may well represent a significant advance in both the safety and training of surgical procedure.
OpenGL and Virtual Reality Modeling Language were used to create precise 3-D mathematical software models based on engineering drawings. The software gives the surgeon the ability to pan, rotate, and zoom to high magnification levels using the two touch-screens, creating an immersive visual environment. A volume accelerator card on the MR display provides 3-D volumetric renderings of the patient’s latest MR images. The two touch-screens show the positions of arms and tools as they update in near real time via telemetry from the manipulator encoders, which provide an accurate and dynamic view of motions being made by the surgeon. Plane cuts at arbitrary positions and angles relative to the tip of the tool, as well as an optional linear tool-tip extension, can be applied virtually. By combining rendered and real video displays, neuroArm allows surgeons to function within both real and virtual environments.
NeuroArm has now been introduced into a neurosurgical operating room that includes an intraoperative MR (iMRI) imaging system based on a 3 Tesla movable magnet (IMRIS; Winnipeg, MB). To perform image-guided microsurgery, the manipulators are spatially registered to the radio-frequency coil, and thus the patient’s head, using the digitizing arm. Various tools allow precise tissue cutting, dissection, cauterization, suturing, and suction. Thus far, various portions of tumor removal have been performed in five patients. In stereotactic mode, cadaver studies have shown accurate registration, with precise biopsy and implantation of ferromagnetic nanoparticles. Clinical studies are ongoing for both microsurgery and stereotaxy to show both the safety and efficacy of the newly developed surgical robot.
Development of neuroArm was supported by grants from the Canada Foundation for Innovation, Western Economic Diversification Canada, and Alberta Advanced Education and Technology. ‹‹
References:
- G. R. Sutherland et al., IEEE Engineering in Medicine and Biology 27, 59 (2008).
- G. R. Sutherland et al., J. Neurosurgery 91, 804 (1999).
- G. R. Sutherland et al., Neurosurgery 62, 286 (2008).
- A. D. Greer et al., IEEE/ASME Trans. on MRI Compatible Mechatronic Systems 13, 355 (2008).
Dr. Garnette R. Sutherland is professor of neurosurgery in the Department of Clinical Neurosciences at the University of Calgary, Alberta Health Services; Jason W. Motkoski and Catherine O. Sutherland are Project neuroArm research assistants, and Alexander D. Greer is a robotics engineer at Project neuroArm at the Seaman Family MR Research Centre, University of Calgary; Calgary, Alberta, Canada. Contact Dr. Sutherland at [email protected].