Adaptive optics technique images the living human eye in detail never before seen
Using adaptive optics (AO), researchers at the University of Rochester (Rochester, NY), Marquette University (Milwaukee, WI), and the Medical College of Wisconsin (MCW; also of Milwaukee) were able to see through the murky distortion of the outer eye, revealing the eye's cellular structureâincluding tiny, light-sensing cells known as rodsâwith detail never before seen. This could help speed diagnosis of degenerative eye disorders, leading to quicker intervention and more effective treatments.
Joseph Carroll of MCW, one of the research team members, says that early detection of retinal disease is key, citing that one of the major hurdles is that by the time retinal disease can be perceived by the patient or detected with clinical tools, significant cellular damage has often already occurred.
Using a noninvasive AO imaging system, research team leader Alfredo Dubra of the University of Rochester and his colleagues were able to push the device's resolution to its optical limits of nearly 2 µm, which equals the approximate diameter of a single rod in the human eye.
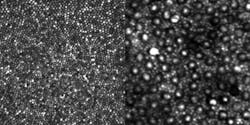
Rods are much more numerous than cones and are vastly more sensitive to light. With the optical design method successfully demonstrated by Dubra's team, even the smallest cone cells at the center of the retina, known as the foveal center, can be seen very clearly. Rods can be seen clearly in a less central retinal location (see figure).
"This is a really exciting breakthrough," says Steve Burns, a professor in the School of Optometry at Indiana University (Bloomington, IN) , who is not involved in the research. "Imaging contiguous rod mosaics will allow us to study the impact of a whole new class of blinding disorders on the retina. Since many of the eye diseases most amenable to intervention affect the rods, this should become a major tool for determining what treatments work best for those disorders."
In astronomy, adaptive optics is able to correct for the blurring effect of Earth's atmosphere, effectively removing the "twinkling" from starlight and rendering cosmic objects as very sharp points of light. To achieve this correction, the AO system requires a reference pointâeither a bright, nearby star or an artificial "guide star" produced in the upper atmosphere by lasers mounted on a telescope. By monitoring that reference point, AO systems use a deformable mirror to create the exact but opposite distortion that is happening in the atmosphere. The result is a clearer image with much greater resolution.
Just as light passing through the atmosphere becomes bent and distorted, so too does light passing through the front part of the eye. This distortion is inconsequential on the scale of human vision, but poses a significant barrier in the microscopic realm of medical imaging.
In 1997, David Williams of the University of Rochester led the group that first demonstrated using AO technology to study the interior of the human eye. In this system, called an adaptive optics ophthalmoscope, a laser creates a reference point that is used to correct the blurring of the image obtained with a fundus camera. Today the fundus camera is commonly replaced by a second laser for imaging, which is known as an adaptive optics scanning laser ophthalmoscope. By moving the laser point across the retina and correcting the distortion along the way, line-by-line an accurate image emerges, in much the same way that a CRT monitor renders an image.
Though earlier AO systems could effectively image cones and have become a mainstay of high-resolution retinal imaging research, the smaller rods, which outnumber cones 20 to 1 in the retina, have eluded clear and contiguous observation in the living eye.
The breakthrough in the design of the AO instrument that led to clearly visualizing rods was, according to Dubra, "embarrassingly simple, and relied on well-known equations and concepts." By simply folding the spherical mirrors that act as lenses in the instrument into a three-dimensional structure, the image quality of the retina was improved sufficiently to clearly resolve the contiguous rod mosaic, as well as the entire cone mosaic at the foveal center.
"By combining careful optical engineering, excellent adaptive optics control, and knowledge of the visual system the authors have made a major advancement in both biomedical imaging and vision science," says Burns.
According to the researchers, their next step is to develop a clinical model that could be widely available. A related task is simplifying and teaching the art of interpreting AO images to guide clinical decisions about diagnosis and treatment.
When that occurs, hopefully in the next 5 to 10 years, doctors will likely be able to routinely peer into a living human eye with such precision and clarity that they will be able to see and evaluate individual rodsâand do three things never before possible: accurately describe the physical presentation of specific rod disordersâthe "phenotype" of a disease, intervene with early treatment at the first sign of disease, and even determine how individual cells are responding to a specific treatment.
"That's what's really exciting about this imaging device: it can really make a difference in a patient's life," says Carroll. "The ability to now resolve these cells opens up new possibilities for improving care that researchers have been anticipating for a long timeâsuch as using the information in these retinal images to aid in targeting, delivering, and evaluating therapies."
-----
Posted by Lee Mather
Follow us on Twitter, 'like' us on Facebook, and join our group on LinkedIn
Follow OptoIQ on your iPhone; download the free app here.
Subscribe now to BioOptics World magazine; it's free!