Respiratory rate (RR) is a key indicator of health. But currently, RR measurement depends on contact methods, with inherent difficulties such as patient discomfort, setup complication, and a tendency for errors related to movement or dislodgement.
When these shortcomings became evident during an audit (which revealed 40 percent of patients were not being monitored), medics at Sheffield Children's Hospital (Sheffield, South Yorkshire, England) approached Reza Saatchi, Ph.D., at Sheffield Hallam University for a solution. Saatchi heads the Medical Electronics Engineering Research Group (MEERG), which develops medical electronics and leads research into contactless respiration monitors.
Saatchi's PhD student Abdulkadir Alkali took on the project to produce the 4FA system. Alkali, a native of Nigeria, named it after the word fofa (pronounced "foo-fa"), which means "breath" in the Fulfulde language of the Fula people.
Starting points
Exhaled air is always warmer than inhaled air, and both affect the temperature of skin around the nose. These fluctuations are evident with a thermal camera, and the locations can be analyzed to understand an individual's respiration pattern.
Because a sick infant's RR can be >80 cycles/min, Alkali aimed to develop a device that would process infrared, thermal images at a stable rate of 25 frames/s, while mitigating the effects of movements (including those caused by heartbeat).
Working with Saatchi, he used LabVIEW (National Instruments, Austin, TX) to develop an application to control operation of a FLIR (Boston, MA) A40 thermal camera. Thus, he was able to control data acquisition, image processing, and feature extraction, and to display the images and RR metrics, with a single application.4FA uses four discrete stages to determine the respiration rate:
1. Image acquisition and subject segmentation
The camera acquires images with help from the NI Vision Development Module and FLIR ThermoVision LabVIEW Toolkit. A high-pass filter removes impulse noise; images are reduced to 8 bits and then segmented to remove all background, leaving just the subject.
2. Face detection and tracking
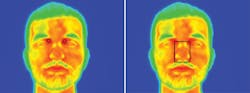
The subject image is further segmented to capture just the face, which is mapped on the original acquired image to indicate detection.
3. Eye corner detection
The corner of one eye (eyes are the warmest points on the face) is located and its value and position enables location of the second eye's corner, with help from an intelligent learning algorithm (developed with the NI Vision Development Module).
4. Nose detection and extraction of RR
The coordinates of the eyes help locate the tip of the nose (the coldest part on the face), and in turn its coordinates help to define a region of interest (ROI): the nostrils below the corners of the eyes. The pixel values within this ROI are extracted and processed as a respiration feature for the frame. The operation is repeated with each incoming frame; then, signal processing calculates the RR.
The 4FA system is now undergoing clinical trials and has increased RR monitoring in child patients by about 50 percent. Future goals for the system include less costly components, a renewable power source, "intelligent" features like an alarm (for when RR exceeds a range), more complete analysis of respiration, and software with diagnostic capabilities.
About the Author

Barbara Gefvert
Editor-in-Chief, BioOptics World (2008-2020)
Barbara G. Gefvert has been a science and technology editor and writer since 1987, and served as editor in chief on multiple publications, including Sensors magazine for nearly a decade.