Photoacoustic imaging could make catheter-based heart procedures safer
In the first study of its kind, researchers at Johns Hopkins University (Baltimore, MD) provide evidence that photoacoustic imaging could someday replace current methods that require potentially harmful radiation.1
The findings detail success in a heart procedure but can potentially be applied to any procedure that uses a catheter, such as in vitro fertilization or surgeries using the da Vinci robot (made by Intuitive Surgical), where clinicians need a clearer view of large vessels. The team was led by Muyinatu Bell, assistant professor of electrical and computer engineering at The Johns Hopkins University, director of the Photoacoustic & Ultrasonic Systems Engineering (PULSE) Lab, and the study’s senior author.
The team tested the technology during a cardiac intervention, a procedure in which a catheter is inserted into a vein or artery, then threaded up to the heart to diagnose and treat various heart diseases such as abnormal heartbeats. Doctors currently most commonly use x-ray fluoroscopy, which can only show the shadow of where the catheter tip is and doesn’t provide detailed information about depth. Additionally, Bell adds, this current visualization technology requires ionizing radiation, which can be harmful to both the patient and the doctor.
In photoacoustic imaging, energy from a pulsed laser piped to an area in the body is absorbed by photoabsorbers within the tissue, such as the protein that carries oxygen in blood (hemoglobin), which results in a small temperature rise. This increase in temperature creates rapid heat expansion, generating a sound wave. The sound wave is received by an ultrasound probe and reconstructed into an image.
Past studies of photoacoustic imaging mostly looked at its use outside of the body, such as for dermatology procedures; few have tried using such imaging with a laser light placed internally. Bell’s team wanted to explore how photoacoustic imaging could be used to reduce radiation exposure by testing a new robotic system to automatically track the photoacoustic signal.
Photoacoustic image feedback for guidance
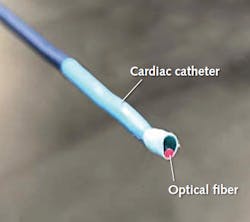
Using the paired optical fiber (with 635 nm light used for visualization and 750 nm light to produce the photoacoustic signal) and catheter (see figure), Bell’s team performed cardiac catherization on two pigs under anesthesia and used fluoroscopy to initially map the catheter’s path on its way to the heart. The team also used robotic technology to hold the ultrasound probe and maintain constant visualization via the photoacoustic signal, receiving image feedback every few millimeters.
Finally, the team looked at the pig’s cardiac tissue after the procedures and found no laser-related damage. While the team needs to perform more experiments to determine whether the robotic photoacoustic imaging system can be miniaturized and used to navigate more-complicated pathways, as well as to perform clinical trials to definitively prove safety, they say these findings are a promising step forward.
“This is the first time anyone has shown that photoacoustic imaging can be performed in a live animal heart with anatomy and size similar to that of humans,” says Bell. “The results are highly promising for future iterations of this technology,” says Bell.
Source: https://releases.jhu.edu/2020/04/17/lighting-the-way-to-safer-heart-procedures/
REFERENCE:
1. Michelle Graham et al., IEEE Transactions in Medical Imaging, vol. 39, no. 4, pp. 1015-1029, April 2020; doi: 10.1109/TMI.2019.2939568.
Got optics- and photonics-related news to share with us? Contact John Wallace, Senior Editor, Laser Focus World
Get more like this delivered right to your inbox

John Wallace | Senior Technical Editor (1998-2022)
John Wallace was with Laser Focus World for nearly 25 years, retiring in late June 2022. He obtained a bachelor's degree in mechanical engineering and physics at Rutgers University and a master's in optical engineering at the University of Rochester. Before becoming an editor, John worked as an engineer at RCA, Exxon, Eastman Kodak, and GCA Corporation.