NANOTECHNOLOGY/LIGHT ACTIVATION: IR light method turns blood clotting on (like drugs) and off (like nothing else)
Gold nanoparticles, controlled by infrared (IR) light from a pulsed femtosecond laser, promise to promote wound healing and help doctors control blood clotting in patients undergoing surgery.1
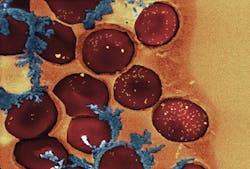
Blood clotting results from a long chain of protein interactions, which eventually form fibrin, a fibrous protein that seals wounds. Heparin and other blood thinners interfere with this process by targeting reactions that occur during the blood-clotting cascade, but reversing the effects of such drugs requires removing them from the bloodstream. A better solution, says Kimberly Hamad-Schifferli, a technical staff member of the Lincoln Laboratory at the Massachusetts Institute of Technology (MIT; Cambridge, MA), is an agent that targets only the last step: the conversion of fibrinogen to fibrin.
This last step is a reaction mediated by an enzyme called thrombin. Earlier research showed that DNA with a specific sequence inhibits thrombin by blocking the site where it would typically bind fibrinogen. The complementary DNA sequence can shut off the inhibition by binding to the original DNA strand and preventing it from attaching to thrombin.
Hamad-Schifferli and colleagues had previously demonstrated that gold nanorods can enable the release of drugs or other compounds when activated with IR light, and the size of the nanorod determines the wavelength of light that will activate it. To manipulate the blood-clotting cascade, she decided to load a 35-nm-long nanorod with the DNA thrombin inhibitor and 60 nm rod with the complementary DNA strand. But the researchers found they couldn't load enough DNA onto each particle to make this process effective. By soaking the nanorods in a solution of human serum protein and the DNA molecules, however, they found they were able to attach six times more DNA than through chemical bonding. Now, when the nanorods are exposed to the correct wavelength of light, electrons within the gold melt slightly and release their DNA payload.
In tests using donated blood, the researchers found that the particles successfully turned clotting on and off in all samples. But to make the particles practical for use in patients, they would need to be targeted to the site of injury, which the researchers are now working on doing. Once they reached the site, they would need to be within a few millimeters of the skin surface for the IR light shone on the skin to reach them.
The researchers are also working to modify the system so particles can be activated using a continuous-wave (CW) laser, which is smaller and less powerful than the laser they are currently using.
1. H. de Puig, A. Cifuentes Rius, D. Flemister, S.H. Baxamusa, and K. Hamad-Schifferli, PLoS ONE, 8, 7, e68511 (2013); doi:10.1371/journal.pone.0068511.