Laser advancements offer pain-free aesthetic treatments
Lasers have become a valuable tool for hundreds of medical applications. Within a year of the introduction of the first laser—a ruby laser developed in 1960—it was commercially available and used in surgery. The adaptation of lasers for medical procedures quickly evolved given their ability to focus to very high-power densities in sterile (noncontact) processes, coupled with the potential to provide cauterization.
Specific lasers for medical applications are chosen for their power and wavelength and the interaction and penetration with tissue. Earlier devices such as CO2 lasers did not have compatible fiber optics and required the use of articulated arms with multiple mirrors for delivery and manipulation of the laser beam. Today, the majority of medical laser devices can be coupled to fiber-optic cables that are flexible, lightweight, and easily manipulated by the practitioner. With such ease of use, lower risks, and noninvasiveness, we can now find almost every type of laser in use by surgeons, dermatologists, dentists, and veterinarians.
Patients are opting out of surgical procedures for newer technologies using lasers that offer much lower risk and excellent results. In the field of plastic surgery and cosmetic treatment, the term “body sculpting” has been applied to procedures that are noninvasive and void of post-treatment recovery time, and can be applied to wrinkle removal, fat reduction, and muscle toning.
All living cells go through continuous cycles of division or growth and death. Apoptosis is a continuous normal cell death, which is natural and transpires over several weeks. Necrosis is sudden cell death that results in biological defense mechanisms, such as permanent scar tissue generation. Properly applied fat reduction relies on apoptosis to the adipose (fat) cells and will occur when these cells are exposed to either cold or hot temperatures. Application of heat from radio frequency (RF), ultrasonic, or lasers creating fat tissue temperatures between 42° and 52°C results in apoptosis. Tissue temperatures above 52°C are associated with necrosis and undesirable side effects and must be avoided.
The 1064 nm diode-pumped laser has been found effective in fat-removal and other similar applications, as it is capable of penetration into the subcutaneous fat tissue (see Fig. 1). Wavelengths near 1000 nm have relatively good transmission through the skin and dermis tissue, which can be characterized by H2O, hemoglobin, and melanin. Furthermore, wavelengths near 1000 nm have higher absorption in fatty tissue. Dominion Aesthetic Technologies (Houston, TX), for example, has discovered the efficacy of the 1064 nm Nd:YAG diode-pumped laser for pain-free body sculpting aesthetic treatments with zero post-treatment recovery time.
Traditional Nd:YAG laser devices were flashlamp-pumped and required circulating water cooling systems. They function well and provide the desired laser properties. However, they are typically less than 5% efficient and normally include circulating water cooling and maintenance. Using diode lasers to replace the flashlamp increases the efficiency but normally still requires water cooling and higher costs. Over the past 10 years, fiber lasers with wall-plug efficiencies approaching 40% are gradually replacing solid-state and CO2 lasers for industrial applications. Since fiber lasers employ fiber-coupled diode lasers as their pump source, this technology has advanced as well; diode laser suppliers have realized that fiber-coupled modules can compete with older industrial lasers for many applications, with their broad range of available wavelengths.
Laser-diode bars operate with low DC voltages in conductively cooled modules that can easily produce more than 50 W of continuous power. Optically combining several diode bars creates compact fiber-coupled laser devices well over 1000 W. With wall-plug efficiencies as high as 50%, conductive or baseplate cooling is possible for output up to 300 W. The choice of a fiber-coupled laser diode module is easily justified by wavelength, compact size, high efficiency, fiber delivery, baseplate cooling, and maintenance-free lifetimes near 50,000 hours. Medical-grade products that include internal temperature and laser power monitoring, fiber sensing, visible aiming beams, and external blow-back windows are now common.
Such technology powers systems such as Dominion’s Eon. With this system, since the laser was baseplate-cooled, a stable heat sink to dissipate the heat was required. Forced convection cooling with high-volume fans became more difficult at higher power levels. Dominion integrated a miniature direct-refrigerant cooling (DRC) system that touts more than 600 W of cooling capacity at 20°C. With the laser fastened to the cold-plate (the evaporator) and graphite thermal gap pad, the laser can maintain its recommended 25°C for safe and reliable operation.
Figure 2 shows the small compressor that is the heart of the DRC chiller (developed by Aspen Systems [Marlborough, MA]). With direct refrigerant or direct expansion cooling, the refrigerant flows directly through the cold plate with the circulation being driven by the compressor. Compared to typical liquid chillers, the advantages are multifold: DRC eliminates the need for a liquid recirculating pump, fluid reservoir, and liquid lines and connectors, which are primary sites of leaks and failures. The efficiency is improved by removing the losses associated with cooling a secondary liquid and energy savings of driving a pump. Systems such as this can provide high reliability (MTBF >100,000 hours) and reduce the size of the cooling system.With the laser and its cooling system defined, the appropriate laser power and beam shape can be created. The laser power from the fiber optic is collimated by a simple plano-convex lens. To avoid hot spots in the tissue, a top-hat diffuser is mated to the collimated beam. A microlens array (MLA) optical element homogenizes the beam, creating a diverging uniform square pattern. In using the Eon system, for example, the beam size on the patient’s skin was controlled by the distance from the MLA to produce the desired power density. During development, tissue heating was tested in a single area; to reach and maintain the desired fat tissue temperatures, the laser duty cycle was relatively low. Here, the laser can remain on and scan over a larger area, still reaching the desired tissue temperatures. This laser beam-scanning approach was solved in this system by mating to a robotic arm.
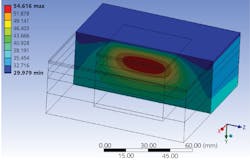
Attaching a laser treatment head to a robotic arm allows a fully automated, noncontact protocol over a large area (see Fig. 3). Robotic controls allow the treatment head to follow the patient’s body contour, while precisely maintaining the correct standoff distance to the skin’s surface. During setup, the visible aiming laser beam produces a red beam pattern for the practitioner to accurately define the treatment zone. The automated protocol runs for 20 minutes as the robotic head and the laser beam follow the pattern with multiple sensors for control and safety.Development of the proper protocol to reach and maintain the target temperature range of 42° to 52°C in the fat tissue requires control of multiple features. A balance between the laser power density, the scan area, the scan rate, skin cooling, and the treatment time must be achieved. In its research to create its system, Dominion developed a tissue model based on finite element analysis (FEA) simulations (see Fig. 4). This model included thermal properties for all the differing tissue layers: skin, epidermis, dermis, adipose, and blood profusion. Using actual tissue test data with embedded thermocouples, the parameters were refined to accurately predict the laser’s tissue thermal interaction. To avoid necrosis, the treatment protocol was carefully developed so the targeted fat tissue would approach and maintain temperatures near, but not over, the threshold for necrosis at 52°C. The efficiency of apoptosis increases exponentially with temperature. Therefore, by reaching consistent higher adipose tissue temperatures, much higher levels of fat reduction are achieved.
In parallel with finding the optimum laser heating profile, the patient’s skin temperature must be cooled to avoid discomfort. The medical consensus for safety is to limit skin temperatures to 42°C. Investigations of differing cooling techniques have included forced convection as well as evaporation with cryogenic fluids. Normal convection has been found to possess inadequate heat extraction, and cryogenic temperatures have imposed unnecessary risks for tissue damage. To maintain skin temperatures below 40°C while applying high laser power, in the Eon system, for example, excellent heat extraction has resulted from a proprietary cold air jet cooling technology. However, a high-volume air pump coupled to a chilled proprietary heat exchanger can provide cooling air near 10°C, which is transparent to the laser beam and can be easily integrated into the robotic arm’s treatment head.
This combination, along with that of the fiber-coupled diode laser with miniature direct refrigerant cooling, top-hat beam profile, and automation are ushering in new standards for higher efficacy and unprecedented safety in laser aesthetics.
John Daly | CTO, Dominion Aesthetic Technologies
John Daly is CTO of Dominion Aesthetic Technologies (Houston, TX).
Rick Slagle | Managing Partner, Technical Solutions Marketing
Rick Slagle is a managing partner at Technical Solutions Marketing (Maynard, MA).