Micro-interferometer speeds detection of dangerous pathogens
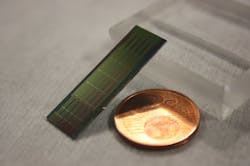
Optical interferometry is the sensitive measurement technique at the heart of such impressive systems as the sprawling Laser Interferometer Gravitational-Wave Observatory (LIGO) detectors, but the same principle also works at microscopic scales. A Spanish research team, for example, is using an interferometric biosensor to rapidly and accurately sense the presence of pathogenic bacteria. The bimodal waveguide (BiMW) sensor is a silicon nitride waveguide with a portion biochemically functionalized to bind to a specific target. Biomolecular binding introduces an effective path difference between two modes, creating intensity variations proportional to analyte concentration, and all in a small package: 20 devices fit on a single 30 × 10 mm chip.
The need for rapid, sensitive detection
Professor Laura M. Lechuga of the Catalan Institute of Nanoscience and Nanotechnology (Bellaterra, Spain) and her colleagues developed their BiMW biosensor in response to the general need for accurate and rapid testing of biochemical compounds.1 Recently, they adapted the device to a specific need: sensing pathogens that cause the $9 billion problem of nosocomial infections, or infections acquired in a hospital or other healthcare setting. Each year, hundreds of thousands of U.S. hospital patients suffer from at least one nosocomial infection.2 Even worse, from 20% to more than 70% of the organisms responsible have some degree of drug resistance.
Current strategies to identify pathogenic bacteria are time-consuming, inaccurate, expensive, or some combination of all three. Lechuga realized the BiMW biosensor could be configured to quickly, accurately, and inexpensively identify these pathogenic organisms or their genetic components.
The BiMW itself is conceptually straightforward. A 350-nm-thick layer of silicon nitride is deposited through low-pressure chemical vapor deposition onto a silicon substrate and enveloped in silicon dioxide cladding. A portion is etched to 150 nm thick, creating a 5-mm-long, 3-µm-wide waveguide, which couples to a 25-mm-long waveguide at the 350 nm thickness.
When a monochromatic polarized beam of visible light is incident on the short waveguide, it propagates in single mode up to the junction of the larger waveguide, which supports both the symmetric fundamental mode and asymmetric first-order mode. Phase differences between the fundamental and first-order beams will create constructive interference with either the top or the bottom lobe of the first-order mode, and corresponding destructive interference in the opposite lobe.
The final stage in device fabrication is to strip the cladding from a 15 mm stretch of the bimodal section. The waveguide-confinement factor is significantly reduced in the stripped region, which enhances the interaction of the evanescent waves with the surrounding medium. The two modes interact differently with the environment through the evanescent field, meaning the interference between the modes is modified as the refractive index of the surrounding medium changes. The trick is then to ensure that refractive index changes in the surrounding medium are linked to levels of the target analyte.
A flexible platform
For example, to detect Pseudomonas aeruginosa, which is responsible for 11% of the nosocomial infections, the sensor surface is biofunctionalized with antibodies specific to antigens in the bacterium membrane. To detect methicillin-resistant Staphylococcus aureus (which causes MRSA), an aptamer is bound to the sensor surface, an aptamer that selectively matches a membrane protein specific to MRSA.3 For this whole-bacteria sensing application, the key is to treat the sensor surface to be nonbinding outside of the designed target analytes, because bacteria and other biological compounds tend to adhere on whatever they contact. The approach worked, as the biosensor proved to be insensitive to the presence of non-specific bacteria, while demonstrating a very high sensitivity—as low as 29 colony-forming units per milliliter for the target bacterium.
Different functionalization lets the biosensor detect DNA sequences specific to drug-resistant bacteria.4 With complementary oligonucleotides adhered to the sensing region, bacterial DNA are extracted, fragmented, and denatured, then flowed in solution through the biosensor. The BiMW sensor can sense target DNA quantities as low as 25 attomoles. Just as importantly, sample processing is minimal—and fast as well, with the total measurement taking from 12 to 40 minutes.
The architecture offers future potential for multiplexing, with different surface treatments allowing simultaneous detection of 10–20 distinct analytes. “Our goal,” says Lechuga, “is the detection of biomarkers in real human samples without any type of preprocessing or cleaning steps of the samples, so the biosensor can operate directly with a few drops of any human fluid.”
Lechuga is working on transitioning the device to mass production, and believes such decentralized biosensor technologies will gain much more attention in the post-pandemic world. “This technology provides sensitive, reliable, and selective analysis, while reducing test and therapeutic turnaround times, decreasing and/or eliminating sample transport,” she says. “But more importantly, the devices can operate at the point of need.”
REFERENCES
1. K. E. Zinoviev et al., J. Light. Technol., 29, 13, 1926–1930 (2011); doi:10.1109/jlt.2011.2150734.
2. S. S. Magill et al., N. Engl. J. Med., 370, 1198–1208 (2014); doi:10.1056/nejmoa1306801.
3. J. Maldonado et al., Analyst, 145, 497–506 (2020); doi:10.1039/c9an01485c.
4. J. Maldonado et al., Diagnostics, 10, 845 (2020); doi:10.3390/diagnostics10100845.
About the Author
Richard Gaughan
Contributing Writer, BioOptics World
Richard Gaughan is the Owner of Mountain Optical Systems and a contributing writer for BioOptics World.