Researchers work to refine lser-based psoriasis trwatments
Anyone who suffers from psoriasis-a chronic skin condition that draws its name from the Greek word for "itch"-will tell you that, while not life-threatening, it is painful, persistent, uncomfortable, and often embarrassing. While the cause is unknown and a cure has yet to be discovered, numerous treatments to control the scaling and hyperproliferation of skin cells do exist, even for the most severe cases. However, because psoriatic lesions can return even after long periods of remission, researchers continue to search for more-effective treatments and a cure.
Psoriasis, which currently affects more than six million people in the USA alone, is characterized by red, scaly patches (plaques) most often appearing on the elbows, knees, scalp, and lower back. The plaques result from an overabundance of capillaries in the dermis that increase blood flow in these areas to more than twice their normal rate, prompting accelerated and excessive skin-cell production in the upper layer of skin. Some psoriasis patients (5%-10%) also suffer from related psoriatic arthritis. Current therapies include topical substances (primarily creams), oral medications, ultraviolet (UV) light, or a photochemotherapy combination of psoralen and UV light. The effectiveness of each therapy varies from patient to patient, lasting several months or even years, and each method has its drawbacks, ranging from skin irritation and liver damage to the increased risk of skin cancer with each UV treatment.
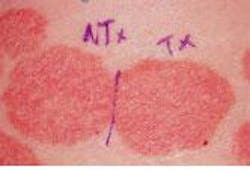
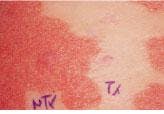
In experimental treatment of a psoriatic plaque with a pulsed-dye laser, each lesion was divided into two parts, with the left side serving as the untreated control and the right side undergoing multiple laser treatments (top). After 11 months of therapy at three-week intervals, the right side of the lesion shows obvious clearing, while the left side remains the same (bottom).
Some of the newest therapies involve lasers and photodynamic therapy (PDT). While lasers have been studied for the treatment of psoriasis since the early 1990s, none have US Food and Drug Administration (FDA) clearance for this application. Some of the earliest work focused on the pulsed-dye laser, which was already being used to treat vascular lesions such as port-wine stains by selectively destroying cutaneous blood vessels. Recognizing that this approach might be successful in targeting the capillary oversupply underlying the psoriatic plaques, Candela (Wayland, MA), Cynosure (Bedford, MA), and some independent re searchers embarked on clinical studies to test out this theory.
One such study, conducted in 1993 by Dr. Brian Zelickson and colleagues at the University of Minnesota Medical School (Minneapolis) and Abbott Northwestern Hospital (Minneapolis), found that a short-pulse, flashlamp-pumped dye laser (585-nm SPTL-1; Candela) could achieve prolonged remission of chronic plaque psoriasis (see figure). Thirty-six patients participated in the study, which compared laser treatment to no treatment in 13 patients and short-pulse to long-pulse laser treatment in 23 patients. The subjects were treated at two- and three-week intervals and followed for up to 13 months; the results were positive enough to prompt further investigation. Significant clinical improvement was seen in 60% of the patients, with no real difference between the short- and long-pulse laser treatments. Those patients who responded to the therapy remained in remission for up to 13 months, and biopsies showed normalization of the blood vessels in the lesions that responded.
"We have shown that the treatment works and that this laser works quite well," says Jim Hsia, senior vice president of research and development for Candela, which is now looking at applying for FDA clearance for this application. "It does seem to attack the vasculature, which seems to send the lesion into remission. We think it makes a very good treatment for localized plaques."
Since that first study, Zelickson and his colleagues have continued to refine this procedure, altering laser parameters such as fluence, pulsewidth, and spot size and adjusting the length of time between treatments. They are also studying vascular patterns in psoriatic plaques to see if they can determine which patients are most likely to respond to the laser prior to treatment.
Other laser approaches
More recent studies have investigated the effectiveness of carbon dioxide, alexandrite, and excimer lasers in treating psoriasis. In a study at Vancouver Hospital and Health Science Centre, University of British Columbia, Canada, for example, Dr. Harvey Lui and
Dr. Mariusz Sapijaszko compared CO2, pulsed-dye, and alexandrite lasers in the treatment of psoriasis.
Ten patients with plaque-type psoriasis had one or two plaques divided into four sections; one section was treated for up to three sessions with the pulsed-dye laser (585 nm, 7 J/cm2, 7-mm spot size, 450-?s pulse duration), one section was treated once with a scanning CO2 laser (6 W, 6-mm spot size, 0.2-s pulse duration), one section was treated up to three times with an alexandrite laser (755 nm, 25 J/cm2, 7-mm spot size, 5-ms pulse duration), and one section served as a nonlaser control. Patients were followed for six months after the first treatment.
When compared to the control section, the dye and CO2 lasers induced significant, long-term improvement of the psoriatic plaques, while the alexandrite laser did not. The researchers also found that only one CO2-laser treatment was necessary to achieve the same results as multiple pulsed-dye laser treatments. Additional studies are planned to assess the role and mechanisms of action of photothermal lasers for this application.
Researchers at Massachusetts General Hospital (MGH; Boston, MA) are taking a different approach with excimer-laser technology developed by Laser Photonics (San Diego, CA) and related methods and technology developed at MGH. Rather than targeting the underlying vasculature, the excimer laser works more like traditional UV-light treatment by preventing the epidermal cells from replicating. However, the laser offers the advantage of being able to more precisely target UV energy on the psoriatic tissue, which means less UV damage to healthy tissue and less long-term risk to the patient.
The excimer laser also causes immunosuppression through local and systemic interactions with the immune system, which contributes to clearing of the inflammation, according to lead investigator Dr. Charles Taylor. In addition, it offers the potential to act as both a diagnostic and treatment device, where the back reflectance of the laser could be used to detect the plaque cells. Laser Photonics and its MGH collaborators believe this approach can reduce the number of treatments needed to obtain clearance or remission, especially in difficult-to-treat areas such as the scalp.
A small clinical study completed last year at MGH demonstrated the ability to clear some plaques for as long as six months with very few treatments and no serious side effects. Results from the study are still being analyzed, however; three additional projects are slated to begin this year.
Photodynamic therapy
Another exciting development in the search for a more successful psoriasis treatment is PDT. Photodynamic therapy lends itself well to this application because it activates selective destruction of hyperproliferating tissues, thus avoiding damage to healthy tissue. Once injected or applied, the photo reactive agent concentrates in the overproducing cells; low-level laser or light energy is then applied, activating free radicals in the membranes of the cells containing the drug and killing those cells. This approach is considered
safer than the traditional psoralen and UV-light approach, which works by disrupting the DNA of overactive skin cells to slow their excessive proliferation.
Dr. Lui at the University of British Columbia is one of the leading researchers in this area. He has worked with QLT Phototherapeutics (Toronto, Canada) and DUSA Pharmaceuticals (Toronto) in studies involving their respective photoreactive drugs and various light sources for treating psoriasis and psoriatic arthritis; many of these studies are ongoing.
In initial clinical trials of PDT using the QLT BPD verteporfin drug and a variety of red light sources-including dye lasers, LED arrays, and fluorescent lamps-Dr. Lui and his colleagues demonstrated that psoriatic plaques can be cleared with local administration of the light and that this approach can decrease inflammatory joint disease. A follow-up study involving 17 patients who underwent weekly doses of intravenous verteporfin and full-body UV-light exposure (310-420 nm) showed that this approach is safe, well tolerated, and holds potential for clinical efficacy. Phase II trials are set to begin. Dr. Lui plans to use blue rather than red light from a fluorescent lamp because of better absorption of the energy by the verteporfin and because blue light is felt to be noncarcinogenic, unlike UV fluorescent light.
Several research groups are now studying the efficacy of orally or topically administering PDT drugs-including verteporfin, DUSA`s ALA compound, and a proprietary drug being developed by Miravant (Santa Barbara, CA)-prior to exposure with a blue- or white-light source (most likely not a laser). These studies are still in the early stages of determining proper dosimetry, light exposure, and other treatment parameters.