Dye turns cancer tissue into lasing medium
Researchers from the University of Utah (Salt Lake City, UT) have discovered that cancerous tissue can be transformed into an optical-gain medium when doped with the dye Rhodamine 6G. The resulting random-lasing effect could prove useful in developing new diagnostic techniques for distinguishing cancerous tissue from noncancerous tissue.1
According to Valy Vardeny, a professor in the university’s department of physics, initial studies demonstrated that when biological tissues are infused with laser dyes, they form feedback systems that make random lasing possible. In addition, by averaging the power Fourier transform (PFT) of the emission spectra across the samples, malignant human tissue can be distinguished from nonmalignant tissue to a spatial resolution of about 2 mm.
Random lasing has been well documented for more than a decade. For example, Robert Alfano’s group at City College of New York (New York, NY) first observed laser action occurring in biological tissues in the mid-1990s.2 Coherent random lasing that leads to a sequence of narrow spectral lines, each corresponding to a coherent emission characteristic, is a more recent phenomenon, however.
“Random lasing is not based on a precise cavity,” Vardeny said. “You don’t fabricate the cavity and put a gain medium in there and adjust the laser. It is a natural phenomenon that exists in a soluble or polymer disordered gain medium. And it turns out that there is coherent feedback for this type of laser that manifests in the gain profile. There are many sharp lines in the gain profile, and each is a coherent mode.”
Proof of random lasing
In early experiments designed to show that random lasing can also occur in biological tissue, Vardeny’s group soaked samples from a potato and a chicken breast in Rhodamine 6G, a laser dye that absorbs strongly in the green and fluoresces strongly in the red. The samples were then pumped with 100-ps, 50-µJ pulses from a frequency-doubled (532-nm) Nd:YAG laser emitting at a repetition rate of 100 Hz. The beam was focused on the sample through a cylindrical lens to form a narrow stripe (100 × 2‑µm) on the illuminated tissue. The emission light was collected using a fiber and sent to a 0.5-m spectrometer with an overall spectral resolution of 0.02 nm.
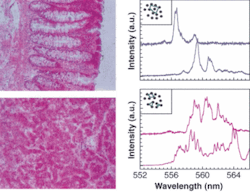
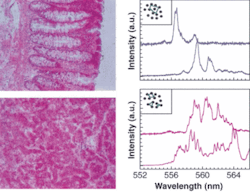
“Above a threshold intensity, this random laser could be observed,” Vardeny said. “So then we tried it in a chicken breast and again saw random lasing.” The same process was then applied to human-tissue samples (see figure).
The next step was to analyze the spectra using PFT; this was done for each collected laser spectrum. The PFT-averaging procedure was done by changing the illuminated stripe on the sample; the minimum lateral change of the illuminated stripe needed to generate an independent spectrum was about 50 mm. The spatial resolution is determined by the size of the laser spot; thus, if 100 spectra are done on a 400-µm spot, 2 mm can be covered in about 10 minutes. Analyzing the resulting data takes an additional five minutes, according to Vardeny. The results, he adds, were surprising.
“By averaging the fully transformed spectrum over the illuminated area, we saw that the average did not smooth out, but rather contains all kinds of harmonics, the same as in a Fabry-Perot cavity,” he said. “And this was a giant step forward.” In fact, they discovered that the harmonics are what distinguish malignant from nonmalignant tissue.
“When we turned attention to two-photon imaging, we found there are more cavities in malignant tissue and many more laser lines,” Vardeny said. “And when you average the lines, in nonmalignant tissue there are harmonics, while in malignant tissue there are no harmonics because there are too many cavities and the average is flat.”
The group is now doing further studies of random lasing with two-photon absorption, and has filed for a patent on this process through the university. According to Vardeny, the goal is to find molecules that have a large two-photon-absorption coefficient for use with IR lasers. In addition, they are looking at other kinds of dyes that are more compatible with live human tissue. He envisions eventually developing a fiber-based in vivo system that could be used during tumor surgery to see whether any malignant tissue has been left behind.
REFERENCES
1. R.C. Polson, Z. V. Vardeny, Applied Phys. Lett. 85(7) (2004).
2. M. Siddique et al., Optics Communications 117, 475 (1995).