Fiberoptic scanning cytometer is fast
Detection of tumor cells in peripheral blood using immunocytochemistry and optical scanning is a promising method for screening and monitoring cancer. But digital microscopy, the current gold standard for sensitivity, is too slow for practical application in diagnostics, and the low specificity requires substantial subsequent examination by a trained pathologist. To scan 50 million blood cells can take more than 30 hours; in addition, thousands of objects in each sample must be reexamined by a specialist to verify the findings.
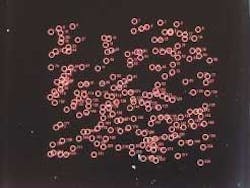
Researchers from the recently formed Scripps-PARC Institute for Advanced Biomedical Studies (La Jolla and Palo Alto, CA) have come up with a laser-based solution that overcomes these limitations. (PARC is Xerox's Palo Alto Research Center.) Leveraging PARC's expertise in lasers, optomechanical engineering, and imaging, the Scripps-PARC team has developed the fiber-array-scanning-technology (FAST) cytometer, which can detect rare cells in as little as two minutes (see figure). The system can also view an area up to 50 mm in size at once, compared to the 1-mm viewing area of digital microscopes.
"Our goal in creating the FAST cytometer is to enable identification of rare cells in the clinic," said Richard Bruce, director of the Scripps-PARC Institute for Advanced Biomedical Sciences and manager of PARC's Computer Science Laboratory. "Because the FAST cytometer uses simple, robust technology and enables cost-efficient operation, we believe it could make screening for cancer or other rare cells as routine as an annual blood test."
The system uses a 488-nm argon-ion laser in conjunction with a fiberoptic bundle to scan cells placed on a slide or surface. Testing begins with conventional staining of occult tumor cells (OTCs) with fluorescent probes. The probes are attached to OTCs through an antibody reaction specific to these cells. The peripheral blood sample is then rapidly scanned for the presence of these probes using the laser.
While OTCs have been found in peripheral blood, their concentration is very low—one in millions. According to the Scripps-PARC team, the key innovation in this work is the asymmetrically shaped fiberoptic bundle that collects the fluorescence. The collection end of the bundle is wide and thin. The laser is rapidly scanned across a sample that is positioned directly underneath the system's 50-mm aperture. The collected fluorescence is transmitted to a collimating-lens system through a small circular aperture at the other end of the bundle.
The collimation is appropriate for conventional optical filtering with subsequent detection in a photomultiplier. The optical-filter system detects two emission wavelengths simultaneously to reduce noise from the staining process. A stage slowly moves the sample across the scanning field. The fluorescent object location can be computed from the position of the stage and laser beam at the time of detection.
The Scripps-PARC Institute is initially focusing on developing tools for structural and functional proteomics. Once probable rare cells are identified, higher-resolution scanning can be used to create images a physician or other qualified expert would review. Cells can also be relocated for additional characterization and testing. The technology has general applicability for other rare cell-related research topics such as the detection of fetal cells in maternal blood and early detection of viral-infected cells.