Blue LED light enables control of insulin secretion
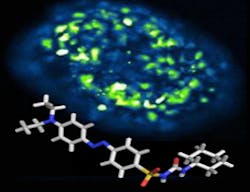
An international team of researchers from Ludwig-Maximilians University (LMU; Munich, Germany) and Imperial College London (England) has incorporated a synthetic, blue light-sensitive molecular switch into a sulfonylurea compound—a class of drugs widely used to regulate blood glucose levels in patients with Type 2 diabetes.
"We utilize synthetic molecular switches whose structure is altered by light in conjunction with the natural receptor proteins for specific signaling molecules," explains Dirk Trauner, an LMU professor of chemical biology and genetics who led the work. "The chemical switches effectively make the receptor's function dependent on exposure to light of a certain color. Light can be controlled with exquisite precision, which allows us to target the receptor of interest with very high specificity. In addition, the activating reaction is itself reversible."
Indeed, it should be possible to control the action of any drug by means of light, opening up novel therapeutic strategies for the treatment of chronic illnesses such as diabetes. Diabetes results from loss of the ability to produce or the capacity to react to insulin, which controls the uptake, metabolism, and storage of glucose by cells. The hormone is secreted by the beta-cells of the pancreas when levels of glucose in the bloodstream rise, and thus serves to keep the concentration of the sugar in the circulation within narrow limits. In Type 2 diabetes, the amounts of insulin released are insufficient to compensate for reduced responsiveness to the hormone. Synthetic drugs called sulfonylureas, which promote secretion of insulin, are therefore used to treat the disease. Trauner and his colleagues have now synthesized a light-sensitive sulfonylurea, called JB253, and tested its ability to stimulate insulin release in laboratory experiments. They were able to show that pancreatic cells incubated with the compound secreted insulin only when exposed to blue light, which converts JB253 into a form that is recognized by its target protein, a potassium channel. Once the light is turned off, JB253 reverts to the inactive form and the effect on the potassium channel and downstream signaling pathways ceases.
The potassium channels targeted by sulfonylureas on the beta-cell surface are open when extracellular glucose levels are low. Rising levels induce uptake and metabolism of glucose, which causes the pores to close, activating insulin release, and sulfonylureas mimic this effect. "Our JB253 prototype could give us an important tool with which to dissect the function of the potassium channels," says Trauner, who also believes that his team's work could have clinical application in the foreseeable future.
The idea is that light-sensitive drugs could be administered in the form of a pill, and then be released or activated by irradiating a patch of skin with a blue LED. When the light is switched off, the drug flips back into the inactive form. "We have a long way to go before it will be possible to use such a therapy in patients. It would, however, give better control over blood sugar levels during type 2 diabetes and would reduce the incidence of side effects, because the active agent is released only where it is required," explains Dr. David Hodson of Imperial College London. The next challenge will be to verify that the new compound JB253 is in fact capable of lowering blood sugar levels in animal models of Type 2 diabetes.
Full details of the team's work appear in the journal Nature Communications; for more information, please visit http://dx.doi.org/10.1038/ncomms6116.
-----
Follow us on Twitter, 'like' us on Facebook, connect with us on Google+, and join our group on LinkedIn
Subscribe now to BioOptics World magazine; it's free!